Introduction
Autologous stem cell transplantation (ASCT) combined with novel agents is considered as the standard treatment for eligible patients < 70(-75) years of age with multiple myeloma (MM). The number of induction cycles is usually 4-6 followed by ASCT, consolidation and maintenance. The role of consolidation is still under debate especially if complete response has been achieved and maintenance will follow. To improve the quality of life and avoid the frequent visits at hospital an all-oral treatment would be a preferred choice. Despite novel drugs, the outcome of high-risk (HR) patients is poor. We designed a phase 2 Nordic Myeloma Study Group (NMSG) trial (NCT03376672) to explore the response of ixazomib, lenalidomide and dexamethasone (IRd) induction, followed by single ASCT, IRd consolidation and risk-based maintenance either with IR or R. Here we present the response rates and safety after IRd x 4 induction in all patients and in 87% of patients before consolidation.
Patients and methods
This study included 120 patients in 22 NMSG sites. Patients received 4 IRd cycles as induction, ixazomib 4 mg on days 1, 8, 15, lenalidomide 25 mg on days 1-21, dexamethasone 40 mg weekly in 28-day cycles. Mobilization and ASCT were performed according to standard practice. Three months post-ASCT all patients will receive 2 IRd as consolidation followed by maintenance. Thereafter patients will be stratified to HR if any of the following FISH aberrations were found at inclusion: del17p at least 60%, t(4;14), t(14;16), t(14;20) or +1q and they receive ixazomib 4 mg on days 1, 8, 15 and lenalidomide 10 mg on days 1-21. Non-HR patients receive lenalidomide 10 mg on days 1-21. Maintenance will continue until progression (PD). Lenalidomide dose will increase to 15 mg after 3 cycles. The primary endpoint of the study is minimal residual disease (MRD) by 8-color Euroflow < 0.01%. The secondary endpoints include flow-MRD negativity by 10-5, overall response, safety and progression-free survival. Serological responses were assessed before cycles and if sCR or CR is achieved flow-MRD sampling will be performed and repeated every 6 months. Samples were taken concomitantly for later comparison with BM- molecular-MRD, blood cell-free DNA, blood heavy-light chain assay and blood mass spectrometry.
Results
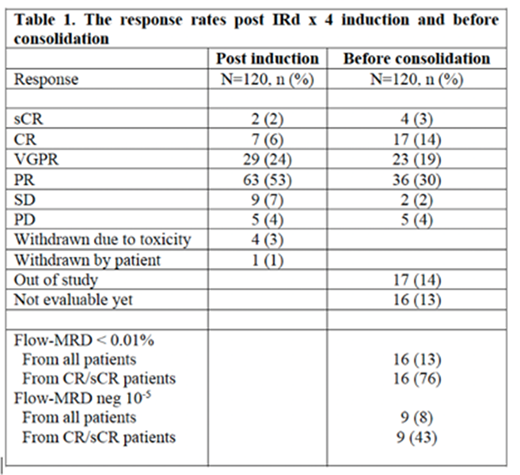
Within 21 months 120 patients were included, 46 % of them belong to the HR group. Mobilization is by July 2020 performed for 101 (84%) patients with cyclophosphamide (Cy) + G-CSF in 74% and G-CSF alone in 26%. Plerixafor was needed in 32 (32%) patients. The median number of harvesting days was 2 (0-4) and the median number of collected CD34+ cells was 6.4 (0-19.2) x 106/kg. Four patients (4%) failed to mobilize during 1st attempt. Eighty-six (72%) patients have so far received ASCT with the median number of 3.4 x 106/kg CD34+ cells in graft. Overall response rate is 93%. The responses after IRD x 4 induction and before consolidation are presented in Table 1.
Before consolidation 10 patients (8%) are out of study due to PD and 4 (3%) have been withdrawn due to toxicity. Toxicity events included hypersensitivity with hepatorenal failure, grade 3 cytopenia with liver toxicity and one unexplained encephalitis. One patient was withdrawn due to Cy toxicity. Eight additional patients are withdrawn from study, 7 by physician´s decision and 1 by patient´s decision. All these 7 patients had high tumor burden based on paraprotein level either in serum (53 - 102 g/L) or in 24h urine (7.8 - 23.2 g/24h) and achieved only stable disease (SD) during induction.
Fifty-eight grade 3-4 SAE reports from 39 (33%) patients have been received and 57% of these were infections. Three patients had grade 3 liver problems and 2 patients grade 3 peripheral neuropathy. Seventeen (14%) patients have reported skin reactions, only 4 of them grade 3 events.
Conclusion We present here data on response and safety after observation of all patients until post-induction phase and of 87 % of the patients until start of the consolidation phase. The ORR is 93% when all patients have received induction treatment. Nine patients achieved only SD and seven of them with high tumor burden were withdrawn before mobilization. At least VGPR after ASCT was achieved in 37%. Toxicity caused the withdrawal of 4 (3%) patients and 39 (33%) patients have reported grade 3-4 non-hematological SAEs. In all, 98/120 (82%) patients continue in the study including 80% of the HR patients.
Silvennoinen:BMS: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Cancer patients Finland: Honoraria; Janssen: Consultancy, Honoraria; Amgen: Consultancy, Honoraria, Research Funding. Waage:Janssen: Consultancy, Honoraria, Speakers Bureau; Takeda: Consultancy; Shire: Honoraria. Schjesvold:Celgene, Amgen, Janssen, Oncopeptides: Research Funding; Amgen, Celgene, Janssen, MSD, Novartis, Oncopeptides, Sanofi, SkyliteDX, Takeda: Honoraria; Amgen, Celgene, Janssen, MSD, Novartis, Oncopeptides, Sanofi, Takeda: Consultancy. Anttila:Sanofi: Research Funding; Amgen: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; BMS: Research Funding; Janssen: Honoraria, Other: Advisory Board; Takeda: Honoraria, Research Funding. Säily:Amgen: Honoraria; Abbvie: Honoraria; Celgene: Honoraria; Roche: Honoraria; Sanofi: Honoraria; Pfizer: Honoraria; Takeda: Honoraria; Janssen Cilag: Honoraria; Boehringer Ingelheim: Honoraria. Sankelo:Celgene, Amgen, Sanofi: Other: Congress travel support. Partanen:Abbvie: Honoraria, Other: Scientific Advisory Board Meeting; Behring: Honoraria; Takeda: Other: Scientific Advisory Board Meeting.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal